|
| The true definitions of euthanasia and assisted suicide versus the euphemisms used by proponents for both |
With the recent release of the parliamentary report, Medical Assistance in Dying: A Patient-Centred Approach, from the Special Joint Committee on Physician-Assisted Dying, it seemed only fitting that with today's post I return to the issue of euthanasia and assisted suicide. Although an important read in of itself, that would help Canadians further understand how the "culture of death" is being ushered into Canada, today's post does not focus on the parliamentary report, but rather on a presentation, The Implications of Legalizing Assisted Suicide, made by Larry Worthen, executive director of the Christian Medical and Dental Society (CMDS).
I was not at the presentation, but I did watch it in its entirety on YouTube. The presentation is thirty-one minutes long, and contains several thought provoking points that spotlight the negative implications of having euthanasia and assisted suicide legalized in Canada. If you are somewhat new to this issue, watching this video will certainly raise your awareness level, and provide you with a greater understanding of what is at stake. You may also want to consider reading my post, Euthanasia - A False Mercy, to bring you "up to speed," on how and why euthanasia and assisted suicide has become such an issue in Canada, and what the teachings of the Catholic Church have to say about it.
The remainder of this post does not summarize the entire video, but rather focuses on selected segments that I found particularly important.
War of Words
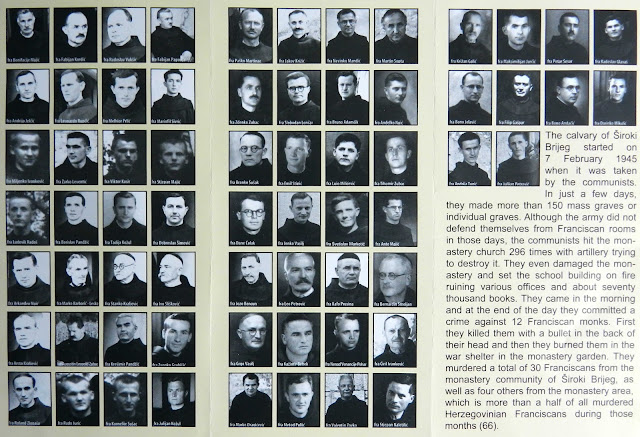
The publishing of the image associated with this post seems to have been a most appropriate choice considering how proponents for euthanasia and assisted suicide are making use of manipulative language, including euphemisms, to alter the thinking of Canadians on this issue. If you look to the actual definitions of euthanasia and assisted suicide, and compare them with the ever growing list of euphemisms used to replace them ("physician-assisted death or suicide," "hastening death," "end-of-life care or options,") to recall the Psalmist's admonition seems most fitting, "Woe to those who call evil good and good evil, who put darkness for light and light for darkness, who put bitter for sweet and sweet for bitter" (Isaiah 5:20)
The "War of Words" comes to us though a variety of sources in the media, and in great detail through policy development by professional medical associations such as the Ontario College of Physicians and Surgeons (CPSO) who I have written about in my post, Professional Obligations and Human Rights - An Anti-Life Policy From Ontario's College Of Physicians And Surgeons, and recommendations from the Provincial-Territorial Expert Advisory Group on Physician-Assisted Dying, whose Final Report, I also blogged about at my post, Ontario's End-of-Life Consultations: The Ushering in of Euthanasia and Assisted Suicide and the Increased Moral Disorder in Canada. The use of manipulative language and euphemisms is typically rampant in these types of documents, which have the potential to diminish, and perhaps even remove the truth about euthanasia and assisted suicide from the hearts and minds of those who read them, providing in the process, procedures and guidelines that all amount to one thing, the attempt to rationalize euthanasia and assisted suicide.
At the fourth minute of the YouTube video, Larry Worthen begins to address the "War of Words" in the public square by stressing the importance of using the proper technical terms. Worthen stated how necessary this was because when people hear assisted suicide or physician assisted death, they tend to think that it means "pulling the plug," but this has nothing to do with it. To clarify further, he included the actual mechanisms that distinguish euthanasia from assisted suicide. Euthanasia normally means giving someone a lethal injection, whereas assisted suicide usually involves providing a lethal prescription that allows the patient to take that prescription at a later time.
Carter vs. Canada Supreme Court Ruling
The presentation actually began with a few points on the Carter vs. Canada ruling, in which the Supreme Court on February 6, 2015 struck down sections 241(b) and s.14 of the Criminal Code that dealt with euthanasia and assisted suicide. Worthen immediately spotlighted a very important point; the mistaken inclusion of "terminal illness" as one of the qualifying criteria for "physician-assisted death." The Supreme Court only mentioned that an illness or condition be "grievous and irremediable." In no way did the Supreme Court include or refer to "terminal illness," yet the opposite was reported by Peter Mansbridge at the Canadian Broadcasting Corporation (CBC).
To be clear, here are the two aforementioned sections of the Criminal Code. The Criminal Code, Part VIII Offences Against The Person And Reputation, under the heading of Suicide - 241. Counselling or aiding suicide states the following, "Every one who (a) counsels a person to commit suicide, or (b) aids or abets a person to commit suicide, whether suicide ensues or not, is guilty of an indictable offence and liable to imprisonment for a term not exceeding fourteen years." In addition the Criminal Code, Part I, General - 14. Consent to death, states the following, "No person is entitled to consent to have death inflicted on him." Together these two provisions do not permit for euthanasia or assisted suicide.
The Supreme Court's Carter decision changed all this when it stated that section 241(b), and s.14 of the Criminal Code has no force and effect to the extent that they prohibit PAD (physician assisted death) for a: competent adult person, who clearly consents, and has a grievous and irremediable medical condition (includes illness, disease or disability), which causes enduring suffering that is intolerable to the individual.
The Supreme Court's Carter decision is a deplorable anti-life decision. Worthen spotlighted this point perfectly when he expanded upon what exactly the Carter decision may actually mean and include, in terms of who would qualify for euthanasia and assisted suicide. He asked the audience to notice how all that is required from the Supreme Court, is that an individual's medical condition be "grievous and irremediable," which by this definition, would permit for a paraplegic or quadriplegic to be euthanized, as well as those with chronic illnesses such as rheumatoid arthritis. In addition, the suffering is not meant to be understood as physical pain, but as a subjective test; that is, what is "intolerable to the individual." Worthen concluded this segment by stating that what we are witnessing with the Carter decision, is a failed public perception of what the legalization of euthanasia and assisted suicide may actually entail.
Seventy-Five Percent of Palliative Care Physicians Oppose Euthanasia and Assisted Suicide
Worthen began this segment of the presentation by listing the countries, and states that currently have legalized euthanasia and assisted suicide. There are five countries that have legalized euthanasia: Netherlands, Belgium, Switzerland, Luxembourg, and Columbia. There are three American states that only have legalized assisted suicide: Oregon, Vermont, and Washington.
Worthen asked, what do the doctors feel about it. Before providing their answers, he noted that seventy-five percent of all palliative care physicians in Canada are opposed to the legalization of euthanasia and assisted suicide, which only begged another question, what do doctors know that we don't.
First, it is difficult to detect a cognitive impairment. What exactly does that mean. A cognitive impairment is when a person has trouble remembering, learning new things, concentrating, or making decisions that affect their everyday life. Worthen points to the example of a friend (Barb) who became depressed due to her lengthy stay in a hospital where she was being treated for arthritis. Was her depression sufficient to keep her from being able to provide consent if she had wanted to end her life. Worthen went on to state that the Canadian Medical Association has stated that it is very difficult to determine when someone is depressed whether or not they are actually able to consent to euthanasia or assisted suicide.
Second, there is a risk of coercion and undue influence. Worthen pointed out that people are vulnerable. Those who are sick, and in need of constant care sometimes succumb to a feeling of guilt; that is, of being a burden to family members. It wouldn't take much for an unscrupulous family member to work on that guilt to the point that, the sick family member may be coerced into consenting to euthanasia or assisted suicide.
Third, in all of the jurisdictions there is a non-compliance with protocol. So no matter what things are put in legislation those protocols are very often not followed.
Fourth, there is the fallibility of prognosis. For example, a doctor can tell you that you have only six months to live, but in reality you end up living for another five-to-ten years. The danger lies in acting upon an incorrect prognosis where the patient consents to euthanasia or assisted suicide.
Fifth, it has been documented in Belgium that life ending acts have been performed without specific requests from the patients. These findings were from a survey in Finders, Belgium were thirty-two percent of patient deaths were performed without a request.
Sixth, physicians have many concerns, one of which is the vulnerability patients experience at the end-of-life, after a traumatic injury or debilitating illness. Worthen provided the example of how anyone at the presentation upon returning to their homes, could experience a serious car accident, the result of which could be the amputation of limbs. Such a development could easily make anyone fall prey to discouragement and depression, such that even though we may be able to legally consent to euthanasia and assisted suicide, we might not recognize that if we could just get through that difficult period, we may be able to adjust, and live a healthy, happy and productive life. This is the problem with euthanasia and assisted suicide; there is a tremendous risk of wrongful death.
Adding to all this is the important point Worthen made with respect to the proper focus for end-of-life care; that is, it is not about pain, but about the lack of access to proper palliative care. Expanding on this, Worthen stated that palliative care physicians inform us that pain at the end-of-life can be dealt with with proper palliative care. In Canada today, the real problem facing Canadians is that only thirty percent have access to appropriate palliative care. Worthen concluded this point with a most noteworthy question, "Are we short-circuiting the need to provide proper palliative care by allowing people to end their lives with euthanasia."
Canadian Medical Association Brief to the Carter Case
At this segment of the presentation, Worthen spotlights an important point regarding the Supreme Court; that is, its failure to understand the reality that doctors face in palliative care. He began by quoting a portion of the brief from the Canadian Medical Association:
The trial judge placed great reliance on the ability of physicians to access the competency of patients requesting medical aid in dying and the voluntariness of their wishes. The CMA submits that the challenges physicians will face in making these assessments have been understated, especially in the end of life care context where the consequences of decisions are particularly grave and in a public medical system in which resource constraints are a pressing issue.Worthen began to translate this portion of the brief by stating that, it is a polite way of the CMA trying to indicate to the judges that decisions that are made within hospital and palliative care contexts are very dynamic, active and turbulent. To further spotlight the lack of understanding from the Supreme Court, Worthen explained that the judges seem to project the environment in which they make decisions on to the medical care system. He elaborated on this point by stating that it is their (Supreme Court) assumption that doctors are making these types of decisions with the same amount of time that judges have, and with both sides being articulated as is the case in a court room, but this is not the case. As Worthen noted, in actual fact doctors are under daily pressure to keep beds clear, and to move people out of hospitals. Worthen shared that doctors he had spoken to are very concerned about the capacity to be able spend the time required with patients to determine whether or not they are consenting to death.
The last note from palliative care physicians that Worthen shared at the presentation was the following:
Pain is rarely the reason patients ask for hastened death--it more often comes out of a desire to control the circumstances surrounding death. Palliative care physicians assure their patients that with current tools and resources, pain and other distressing symptoms can usually be controlled and support provided to ensure comfort and quality of life.The Risk of Wrongful Death
Just after the fourteenth minute mark of the presentation, Worthen introduced to the audience a case of wrongful death. Amongst all the negative implications of having euthanasia and assisted suicide legalized in Canada, this is perhaps one of the worst.
The wrongful death case is about Dr. Tom Mortier, a chemistry professor in Belgium, whose mother, Lieve De Troyer, lived with chronic depression. She became widowed from the suicide of her husband, and whose condition worsened after a long term relationship ended, that only exacerbated her depression. On April 19, 2012, Lieve died by euthanasia with the recommendation of one psychiatrist.
An important point to note here is that in Belgium, a patient requires the recommendation of two psychiatrists, but that requirement was not fulfilled in this case. This fact alone tears down the so-called safeguards that one reads about in documents recommending euthanasia and assisted suicide. My recent post on the Final Report from the Provincial-Territorial Expert Advisory Group on Physician-Assisted Dying, as noted in the War of Words section of today's post, contains several references to "safeguards."
What is even more troubling is the shocking circumstances in which her son, Dr. Tom Mortier, found out about his mother's death. One day Dr. Mortier received a phone call from the hospital asking him to come, and pick up his mother's things. He immediately inquired as to why that was necessary. The answer from the hospital, "Because she was euthanized this morning."
It is not a scenario that anyone in their right mind hopes to confront, but the sad reality is that if euthanasia and assisted suicide are legalized, this is exactly what will happen in Canada. This holds true because of the privilege between a doctor and a patient, even though in Quebec, it is recommended that the family be consulted, there is no legal requirement in Canada to do so.
The Implications For Health Care Professionals
There are many doctors who are seriously considering leaving Canada if euthanasia and assisted suicide are legalized, because they fear they would be forced to provide or procure both, in direct violation against their faith beliefs and conscience. Although the Carter vs. Canada decision did mention that, "The physician's decision to participate in assisted suicide is a matter of conscience and religious belief," (p.132) the problem of ensuring this rests with provincial colleges and legislatures to work out the details regarding: referral, performing, and discrimination for not performing.
Worthen stressed how important that last point is, because in essence what this entails is for organizations such as the CMDS to lobby every provincial college and legislature to ensure Christian doctors can continue to practice.
Time to Fight For Christian Doctors
Worthen's wife is a Christian doctor, and he shared with the audience that many patients have come up to him grateful that they have had the opportunity to be treated by a Christian doctor, after which, he boldly stated, "The time has come to fight to keep Christian doctors." I wholeheartedly agree.
Christian doctors potentially face discrimination with their refusal to perform and procure euthanasia and assisted suicide. Here is the scenario that Worthen presented spotlighting this very point. Once you consider euthanasia and assisted suicide as a "medical procedure," and physicians are being hired for palliative care, there is a very real possibility that the governments and departments of health will eventually be able to claim that if a physician is not prepared to provide all the "medical services," for end-of-life care, then he or she will not be hired for the job. Essentially people will be discriminated against because of their religion.
The reality is that Catholics and Christians alike will face incredible challenges to protect our doctors and their practices. If we value having Christian doctors in our communities, then the ushering in of euthanasia and assisted suicide is a clarion call to all Christians to do something about it.
Doing something about it must first begin with a recognition and understanding that this is primarily a spiritual battle, one that begins with, and is sustained by time spent (on our knees) in front of the Blessed Sacrament. In addition, we must also employ the spiritual weapons of prayer (Mass and the Rosary), and fasting. Last, putting faith into action is also a key component. We the laity, must not remain idle, but do our part with the gifts we have, and fulfill our vocation and mission in the Church and the world (Christifideles Laici), to effectively eradicate euthanasia and assisted suicide from our land.
May Saint Gianna Beretta Molla intercede for all doctors, nurses and medical staff in Canada so that conscience rights may always be protected, and that no one will be forced to perform or procure euthanasia, assisted suicide, and any other threats to the value and inviolability of human life.